Metabolic adaptation to weight loss: Where is the science now?
Metabolic adaptation to weight loss – the phenomenon of reduced energy expenditure during and after a period of calorie restriction, is probably one of the most misunderstood topics related to nutrition and body composition.
Ideas commonly shared include but are not limited to:
- As you diet, your body will adapt to the number of calories you are eating and so you have to reduce calories further as you go. This is often used as an argument for keeping kcal high when dieting; after all, if you start on 1000kcal, where do you go when your body adapts to that?
- The faster the weight loss approach, the greater the adaptation is going to be
- To reverse the adaptation, increase calories slowly
- The more times you diet, rebound, and diet again, the worse your adaptation gets
- Adaptation always happen when you cut calories, so calorie reductions don’t work, so do keto or something
- If you diet you’ll go into starvation mode and gain fat
- Adaptation makes dieting impossible and so dieting doesn’t work, therefore you shouldn’t try
I could go on.
What this means is that we have two separate problems: first, when the topic of adaptation comes up people talk past each other because they interpret the term completely differently and so talk about different things, and secondly, at least some of these people are probably interpreting it incorrectly.
Part of the reason for the confusion is that, actually, the idea of metabolic adaptation to weight loss isn’t as clear-cut and well understood in the scientific community as most seem to think it is. Regardless of their interpretation, metabolic adaptation is discussed as some kind of absolute inevitability for everyone who starts to diet by anyone who mentions it regularly, and so one of my intentions with this article is to explore what currently IS known about adaptation, it’s magnitude, and the chances that it would affect you personally or your clients. The first thing I need to do, however, is to outline exactly what adaptation is, and for that we can look back to the now famous Minnesota Starvation Trial conducted by Ancel Keys and colleagues between 1944 and 1945. Note that while these data are very old they are still considered some of the most reliable and useful in the field of starvation due to the depth of analysis and excellent study design.
The design was relatively simple, 36 conscientious objectors to WWII had their calorie intake reduced from around 3200kcal to around 1560kcal using foods likely to be available during the time (the diet was pretty low in protein). This was maintained for 24 weeks, during which time each man was required to walk 35km per week and complete work tasks. The goal was to reduce their bodyweight by 25%, so slightly over 1% per week.
During and after this process a lot of data were collected, helping researchers in a number of fields including that of eating disorders to the modern day, but for our purposes we need to look at their metabolic rates. As would be expected the total daily energy expenditure (TDEE) of each man was reduced, but this is where the first important detail comes in.
When you lose weight you lose tissue, and you become lighter so easier to move around – both of these factors result in a reduction in energy requirements. This makes immediate sense, a 60kg person requires fewer calories per day than a 100kg person assuming similar activity levels, and so the fact that their calorie needs reduced after 25% weight loss should come as no surprise. Not only that, but these individuals will be lethargic thus move less, and so their TDEE will of course go down somewhat.
35% of the reduction to basal metabolic rate, however, (equal to around 180kcal per day) was not associated with reductions in lean body mass or fat mass, and because we’re looking at BMR that means that activity isn’t relevant here either (1). In short, 35% of the reduction in BMR (which represented roughly a 15% reduction overall) was not explained by lost tissue, this was adaptation.
Metabolic adaptation, therefore, is the reduction in basal metabolic rate seen in individuals who are losing or who have lost weight, that is not explained by their lost tissue – and make no mistake tissue will be lost. During weight loss approaches fat, muscle, and a surprising amount of highly energy expensive organ mass will be lost (1), all of which are metabolically expensive. In one study, for example (2) masses of heart, liver, and kidney decreased by 8, 4, and 6%, whereas skeletal muscle (i.e., a lowâmetabolic rate organ) only decreased by 3%, with these changes making up 60% of the change in resting energy expenditure pre to post diet due to how much energy each tissue type requires. On top of this you of course experience muscle loss and then what is left over is your metabolic adaptation.
In short metabolic adaptation is not just the difference between your total daily energy needs pre and post diet, it is the difference between your basal metabolic rate after the diet, and the basal metabolic rate that would be expected in someone of your height, weight, and body composition (including organ mass). That makes it a lot harder to quantify than most realise, and as you will see, a lot harder to predict, too.
It’s not entirely clear just why this adaptation appears, though the hormones leptin and T3, sympathetic nervous system activity and changes in cellular functions (slowed protein turnover, increased mitochondrial efficiency) all seem to contribute (1).
So that’s all interesting and nice, but you’re not reading this blog because you’re interested in the metabolic rates of some guys in the ’40’s, nor are you particularly fascinated by the size of a person’s liver or mitochondrial efficiency. The two questions surrounding metabolic adaptation to weight loss from a practical perspective are these:
- How likely am I to experience adaptation to a given weight loss approach?
- How much adaptation are we talking?
The answer to the first one will allow you to select your fat loss approach in a manner that minimises your risk of adaptation, and the second will then let you plan ahead and reduce your calorie intake accordingly – right? Well, hypothetically that’s true but herein lies the problem: the honest answer to both of these questions is “we don’t know”. Let me explain.
First we have the issue of determining when you’re supposed to measure any adaptation that exists. A recent study took a number of overweight individuals and mapped their resting and total energy expenditure to their fat mass and fat free mas, then used these measurement to predict their resting and total energy expenditure during and after significant weight loss following bariatric surgery. Adaptation was seen at 6 months while weight was being lost, but this had normalised at 24 months after their weight had stabilised (3) indicating that adaptation did occur but that it was only there while weight was actively being lost.
This matches other similar work which found adaptation after 6 months that dissipated after a year, but is in complete disagreement with a study on participants from The Biggest Loser TV show (3). In that study participants lost a similar amount of weight in a similar timeframe to the people who had undergone bariatric surgery in the two aforementioned experiments, but in this cohort adaptation persisted 6 years after weight loss occurred, despite a 60% weight regain (3). To add more confusion, and to quote Hall et al (3):
“Previous studies have found persistent metabolic adaptation 1 year or more after bariatric surgery or diet-induced weight loss after body weight had stabilised. Others failed to detect significant metabolic adaptation after achieving a stable lower weight, and a large recent study suggested that [resting metabolic rate] adjusted for body composition was slightly higher 1 year after [bariatric surgery]”
This all indicates that while it may be the case that most literature seems to find some degree of adaptation present during weight loss (indeed it does seem to present in most studies that look at this), there is no scientific consensus as to whether this persists after weight loss has occurred. This variation may be due to differences in the protocols used (surgery vs diet and exercise, with surgery seeming to come out as preferable – despite what I wish was the case) or differences in what the participants actually do; for example in the Biggest Loser study the participants continued with very high activity levels post-diet which may have paradoxically reduced their resting metabolic rate. The honest truth is that right now it’s not wholly clear whether a person will experience adaptation post-diet, or whether it is something they will only experience while the diet is happening.
The time that it takes adaptation to start occurring is a little better defined. In the Minnesota trial it took 4 weeks for adaptation to start occurring, with the maximum adaptation appearing after a loss of 10% bodyweight (which took 12-20 weeks depending on the participant). Later studies found a similar time course, leading Müller and BosyâWestphal (1) to conclude that in order to create a state of adaptation calorie restriction needed to be continued for at least two weeks – which has promising consequences for those who prefer intermittent rapid weight loss approaches such as that explained on the BTN Advanced Nutrition Coaching Course – Active IQ Level 4. This also falls in line with other work which has found, for example, that three days of complete food abstinence actually increased, rather than decreased, metabolic rate (4).
So we have determined that adaptation happens some time after at least two weeks of calorie restriction (it may take longer) and that it may or may not persist after bodyweight has stabilised post-diet, but how much adaptation is likely to occur?
Again findings vary, though in line with the Minnesota experiment which found a 15% adaptation the aforementioned Biggest Loser trial saw adaptations in resting metabolic rate of up to 18% when body composition was accounted for (5). Similarly the Biosphere 2 experiment (which was a fascinating idea – basically trying to see if people could live in a closed ecosystem) saw a reduction in resting metabolic rate adjusted for body composition of 10-15% after chronic underfeeding (1), but other studies found more modest numbers.
The CALERIE study which involved a 25% calorie deficit for 3-6 months found a reduction in TDEE of 6%, for example (6), and similar adaptations (5-7%) seem to be the most common findings (1). Taken together these data suggest that adaptation, when it occurs, seems to amount to between roughly 5-15% of resting metabolic rate, or roughly 50-180kcal per day total.
That part – ‘when it does occur’, is crucial here, because as it turns out your chance of experiencing adaptation is difficult to predict.
Müller and BosyâWestphal (1) describe three protocols that differed significantly in their design.
- A 12 week diet-induced weight loss protocol in 85 overweight and obese patients consuming a formula-based meal replacement
- A 6 month study looking at 17 bariatric surgery patients
- A 3 week metabolic ward study (the gold standard for controlled nutrition experiments) in 8 normal weight men eating a 50% calorie deficit
On average, resting energy expenditure decreased with weight loss, and when adjustments for fat free mass were made this remained significant. After adjustments for fat mass were made, however, only the three week metabolic ward trial participants were still shown to demonstrate a degree of true metabolic adaptation on average (figure 1).
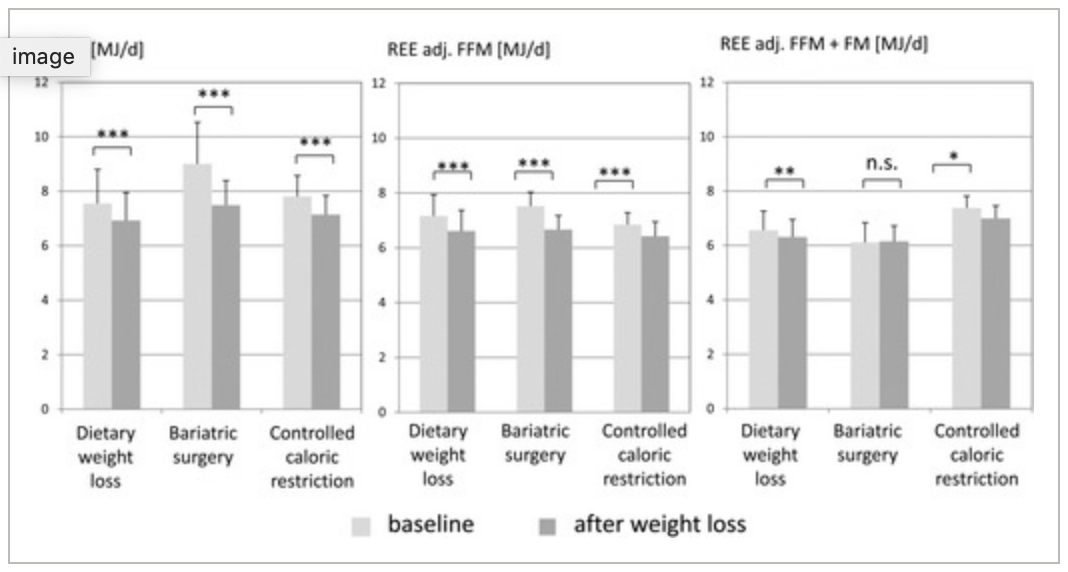
This is not the end of it, however, because this is only an average figure! The prevalence of adaptation in each cohort was 50% (dietary weight loss), 25% (bariatric surgery) and 40% (the metabolic ward trial) meaning that only up to half of the participants actually experienced any adaptation! This means that while it was only the metabolic ward participants who experienced adaptation on average, that is not to say that no adaptation was seen for some individuals in the other protocols – indeed when you look at the individual data the longer term dietary weight loss and bariatric surgery participants both experienced more adaptation than those in the metabolic ward trial (figure 2).
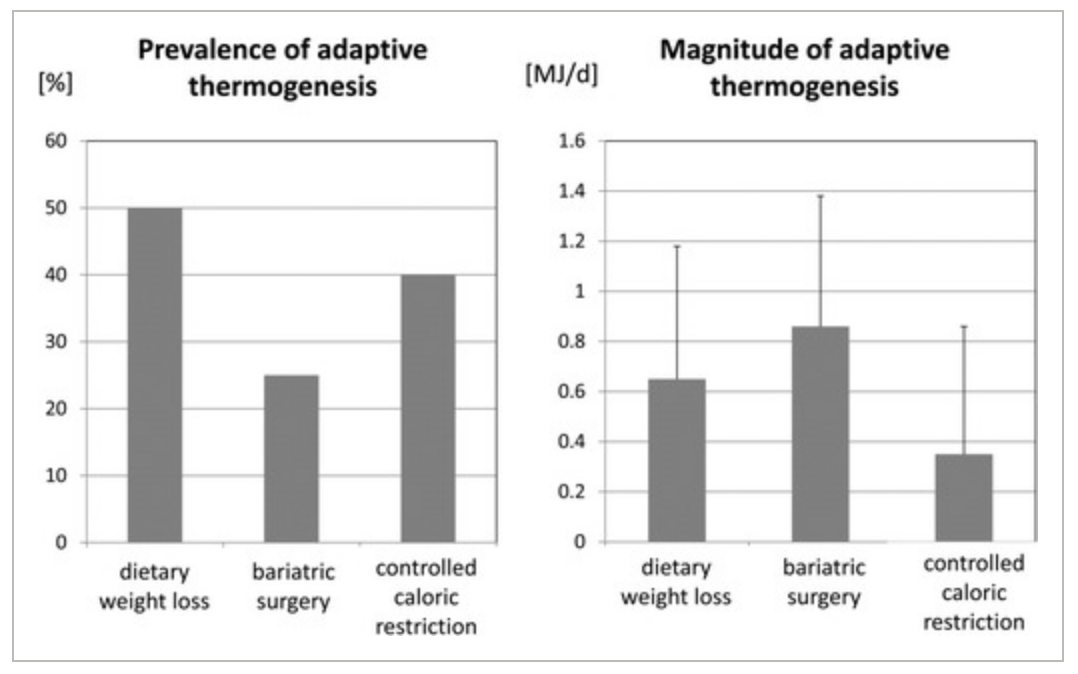
* One megajoule (MJ) is roughly 240kcal.
As an important final note here, because most of these studies have been done on men only, the influence of sex on your chance of experiencing adaptation and the magnitude of the adaptation you are likely to find is not entirely known. As leptin is one hormone implicated in the expression of adaptation, it’s not unreasonable to assume that there may be a sex difference in adaptation, because women carry more fat mass and thus produce more of this hormone (1). That is not to say that NO studies have used women, however, the above mentioned CALERIE study had both men and women consuming roughly a 25% calorie deficit for 6 months and found no difference between the sexes in terms of adaptation (6) which amounted to around 6%.
So what can we take from all of this?
During weight loss your total daily energy expenditure will decrease. You will become lighter and you will lose some metabolically expensive organ, and possibly muscle mass along the way if your weight loss is significant. On top of this you will potentially move less due to diet induced lethargy. This is not all that surprising, and by minimising muscle mass loss, having realistic expectations of what your new maintenance calorie requirement will be, and intentionally keeping activity levels moderate you can counteract much of the effect. What remains is a reduction in your resting metabolic rate which is referred to as true metabolic adaptation.
This adaptation seems to occur in some people but not others, when it does occur it can vary in magnitude, and while in some studies it persists after the dieting phase in others it does not. What is clear, however, that the maximal adaptation ever seen is roughly 18% (the Biggest Loser) while the average is between 5-15 (up to around 180kcal per day), with most studies finding adaptation in the single digits. This happens after at least two weeks of dieting, and the higher adaptation rates only seem to occur after 3-6 months of dietary restriction. Interestingly the MATADOR study published in 2018 (7) found that repeated rounds of two week diet/two week maintenance for 30 weeks achieved the same rate of weight loss as a 16 week continuous diet but with a much reduced level of adaptation, though far more work is needed in this area to be able to say for certain that this is a viable approach.
All in all it seems that if adaptation does occur it will amount to up to 180kcal beyond that which is expected, and more than likely it will be around half this figure. There is no guarantee that adaptation will occur, however, and while there is a general trend towards larger calorie deficits creating greater levels of adaptation there are still no real ways to predict your risk. Even if adaptation does occur, however, it’s not likely to be large enough to prevent weight loss or cause weight gain – though adaptation along with the other factors such as weight loss and reduced activity just might create a halt. Because of this, the best approach is to think only about the adaptations you CAN control by keeping your daily activity up and making sure your kcal intake is appropriate for your weight, and not worrying about adaptation at all.
After all, so far as we can tell the only way to avoid adaptation completely is to not diet in the first place…
References
- Müller, M. and Bosy-Westphal, A. (2013). Adaptive thermogenesis with weight loss in humans. Obesity, 21(2), pp.218-228.
- Lagerpusch, M, BosyâWestphal, A, Kehden, B, Peters, A, Müller, MJ. Effects of brief perturbations in energy balance on indices of glucose homeostasis in healthy lean men. Int J Obes 2011; 36: 1094â 1101.
- Hall, K. (2018). Metabolic Adaptations to Weight Loss. Obesity, 26(5), pp.790-791.
- Zauner, C., Schneeweiss, B., Kranz, A., Madl, C., Ratheiser, K., Kramer, L., Roth, E., Schneider, B. and Lenz, K. (2000). Resting energy expenditure in short-term starvation is increased as a result of an increase in serum norepinephrine. The American Journal of Clinical Nutrition, 71(6), pp.1511-1515.
- Johannsen, D., Knuth, N., Huizenga, R., Rood, J., Ravussin, E. and Hall, K. (2012). Metabolic Slowing with Massive Weight Loss despite Preservation of Fat-Free Mass. The Journal of Clinical Endocrinology & Metabolism, 97(7), pp.2489-2496.
- Heilbronn, L., de Jonge, L., Frisard, M., DeLany, J., Larson-Meyer, D., Rood, J., Nguyen, T., Martin, C., Volaufova, J., Most, M., Greenway, F., Smith, S., Deutsch, W., Williamson, D., Ravussin, E. and Pennington CALERIE Team, f. (2006). Effect of 6-Month Calorie Restriction on Biomarkers of Longevity, Metabolic Adaptation, and Oxidative Stress in Overweight Individuals. JAMA, 295(13), p.1539.
- Byrne, N., Sainsbury, A., King, N., Hills, A. and Wood, R. (2017). Intermittent energy restriction improves weight loss efficiency in obese men: the MATADOR study. International Journal of Obesity, 42(2), pp.129-138.